OK, Semila, you did indeed get my attention! I posted a more limited answer on AuntMinnie due to restrictions on the size of individual responses, but here it is a bit more fleshed-out.Has anyone other than me concluded that the PACS market in general has become a big yawn? The conversations on these boards has deteriorated into techie minutia and nothing exceptional has come from any of the major PACS vendors in recent years. Price erosion continues to dampen the market and no new entries have come into the space in the past couple years. PACS has become a "cog in the wheel". Digital Imaging will in most cases now, be sold with larger information systems and will be a module that can be "turned on or off". PACS is not radiologies baby anymore, but one of the many niches that will make up the EMR/EPR. Aunt Minnie would be wise to diversify the content of its site to begin including more foward thinking discussion.
and
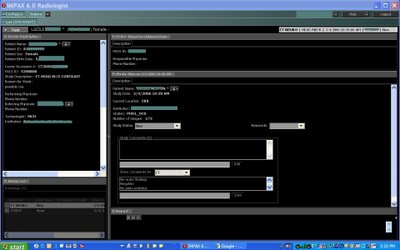
. . . PACS genrerally has one purpose: receive images from modality, compress, store, display and distribute. This isnt rocket science folks, and other industries do this all the time, they just dont have to answer to HIPPA! The foward thinking focus here should be how PACS fits into information systems. The small markets adoption of PACS is irrelevant.
Another note: I for one am a fan of image interperetation being taken away from radiologists and infused into the doctorate programs of the "real" docs, like cardiologists. Doctors that sit in dark rooms or in front of computers providing varying degrees of experience in diagnosis without ever actually seeing a patient is beyond me (teleradiogy - ugh). I am sure I touched a nerve with this one, but c'mon.........really. How bout this Dalai Lama cat.........this guy sounds more like an IT person than a doctor. Scary.
Gee, where do I begin.... First off, I'll take the IT comment more as a complement than anything else, although I am no doubt considered a "scary cat" by both IT and physician camps. I'm in progress on my next AuntMinnie article concerning this particular relationship, and it is guaranteed to touch some nerves. As it turns out, I have degree in Electrical Engineering, major in Bioengineering, minor in Computer Science, so I do have the ability to “talk the talk” of IT, and occasionally even to “walk the walk”.
I tend to agree with semila to some degree about the level of "rocket science" or lack thereof in PACS. It has indeed been commoditized and often just comes as an added bonus with a suite of scanners or other computer systems. Rather like a prize in a cereal box. As an engineer, I do keep in mind that PACS at its core is simply the movement of image data from place to place, and this is not “rocket science” in this day and age. Semila points out that HIPAA plays a major part in its function, but as I found in researching my last article, one can use HIPAA as a template, and not hide behind it to avoid doing your job as some IT folks are wont to do.
At this point, I am going to throw in something so obvious, yet so obnoxious, that it will certainly generate some nasty commentary. So be it….. PACS EXISTS for the radiologists. Ha! Try to disprove that. As Pacs_Guru says, we radiologists are now blind without IT, but IT has no reason to exist without us. PACS defines how I do my job, which is to interpret radiographic and related imaging studies. Without PACS, the patient would still get the study and get it read, but this process would utilize film or perhaps reading directly off of the scanner’s monitor. There is a lot of technical jargon involved in the processes of “receiv(ing) images from modality, compress, store, display, and distribute”, even if it is pretty mundane. Those of us who come here are interested in these “boring” things, and they need to be discussed.
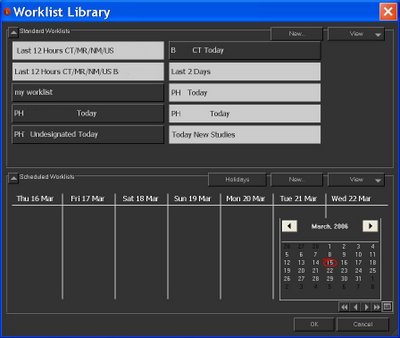
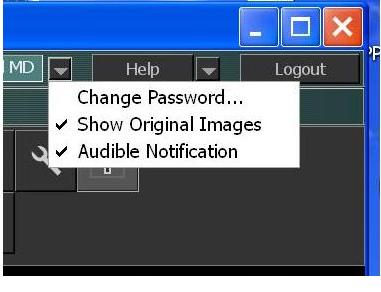
No doubt there will be eventual incorporation of PACS into the wider information systems; we are seeing that already to a minor degree. But since PACS is a tool for radiologists, I will push the very biased view that its next evolution/revolution needs to be in radiology workflow. I have only a vague idea, personally, of where that needs to go. When I went into private practice, 16 years ago, the work model was not so very different than it is today. We would pile in at 8AM, grab 20 or 30 jackets off a stack of 100 or so, put the films on the viewer, interpret them by dictating into a tape-recorder, with demographic information, history, etc, from a paper requisition, take the film down, sack it, stack the jacket, and then do the same for the next patient. The workflow today is to some extent an electronic version of the film days. We sign on to the PACS, select the appropriate worklist, queue up the first study, dictate it into the tank (eventually to VR), using demographics gleaned from the HIS/RIS system, and push the button removing this exam from the list and queuing up the next. (The sweat-shop/factory analogy is apt much of the time.)
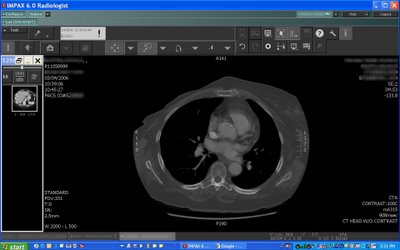
The real difference between film and PACS is that we can manipulate the images we view, and in the case of multislice CT, we can add a number of tools to the armamentarium, including cine-view and the various flavors of 3D such as MPR, Volume Rendering, Virtual Endoscopy, and so on. At some point, there will be some radically different paradigm for reading, although it would have to go hand-in-hand with advances in imaging technology as a whole. We are already seeing that to some extent with whole-body CT. Instead of an X-Ray here and there, our patients are being scanned from head (almost) to toe. There is a great push in this direction from the ER, which wants us to do all their diagnosis for them. Thus, our trauma center often orders “Man-Scans” including CT’s of the head, neck, chest, abdomen, pelvis, total spine, at least one extremity, CT PA gram, and CT Aortogram. One stop shopping, folks. Much as I resent doing the ER’s docs’ thinking for them, I realize that this is where we are in 2006, and somehow my workflow needs to incorporate this monster. Here is where a good, unobtrusive PACS system can help me. All of the imaging needs to be delivered to me in a way that I can read it as efficiently as possible. How about the exams that benefit from 3D (Aortogram, spine CT’s, etc.) being automatically displayed with the MPR’s or VR’s necessary for rapid interpretation? How about automatically displaying relevant priors, images, lab data, etc? That is just the tip of the iceberg, and there are many folks much smarter than I am out there working on all this.
Semila proposes that radiologist need not be the masters of imaging, that other specialties could do at least as well at it. I’m trying very hard not to take this as an attack on my profession, but that is quite difficult as you might imagine. I am assuming that semila is not from the US based on his/her diction, and perhaps things are different is his/her native land. I cannot put it better than did James P. Borgstede, M.D., head of the ACR, in his article “Chipping Away at Imaging” in this month’s Journal of the American College of Radiology:
One of the first canons radiology residents learn when they enter training is to look at the entire image. We are taught that this precept separates us from other physicians who view, but do not interpret, images. Image interpretation, as we all know, is difficult. Sometimes we’re given histories, and occasionally, we even have the opportunity to talk with referring physicians to assist us in our interpretations. Both written histories and dialogues usually focus on clinicians’ suspicions from their histories and physical examinations, assuming they have performed them. Clinicians direct our attention to parts of images or to certain organ systems. By adhering to the first tenet of radiology, we avoid missing unsuspected, but significant, findings included in studies. How many times is a computed tomographic scan requested for pulmonary embolus only to find that the patient has a rib fracture or subdiaphragmatic process that accounts for his or her symptoms? Radiologists, looking at the entire image, hopefully detect the significant abnormalities that are commonly missed by our clinical colleagues only looking at the portions of the studies piquing their clinical interest. These nonradiologist “viewers” of images mentally chip away at imaging examinations, excluding the areas they perceive as irrelevant. By viewing examinations with tunnel vision, they miss significant observations. It seems today that chipping away at images, and in fact our entire specialty, is an avocation of many individuals and groups inside and outside of medicine.Clinicians are keen on focusing on the parts of images within their specialties or subspecialties. Computed tomographic scanners have even been created to assist them in carving away unwanted portions of images. Cardiac imaging is one example; scanners have been created that remove everything from images except the heart. Therefore, physicians focused on the cardiac portions of scans do not have responsibility for the distractions created by bones, soft tissues, lungs, and other mediastinal structures. The companies marketing such scanners emphasize to nonradiologists the freedom from liability and responsibility such scanners create: “If you can’t see it, you don’t have any responsibility for it.” The companies in turn market the same products to radiologists under the pretext of protecting radiology for radiologists by excluding the ability of others to view portions of images that, in the companies’ opinion, are the purview of radiologists. What a help these companies are in chipping away at the images! Unfortunately, patients suffer in this scenario because they may require repeat scans to look at the structures excluded from the original examinations.
The point is that radiologists are trained for many years to interpret the entire image. Remember, what we are looking at is ultimately the anatomy and pathology, not just an image of shadows and density distributions, or water mappings, or areas of glucose uptake. The total yield is definitely more than the sum of the parts here. It doesn’t matter if they are reading a film, a digital image, or holding the patient up to the light. That is why the “old” radiologists are just as good at the new modalities.
Could you train a cardiologist to spot a lung cancer on a coronary CTA? Could you train an orthopedic surgeon to see that same lung cancer on a thoracic spine series? Probably. These folks are very smart and dedicated to what they do best. I mean to take nothing away from them. But where does this mentality stop? Why shouldn’t the surgeon look at the cytopath slides from his biopsy? Maybe he should supervise anesthesia as well? I’m sure he could be trained to do so.
Rather like pathologists, radiologists are impartial arbitrators. We have nothing to gain by coming to one conclusion or another. Once the study is ordered, we have only the goal of finding the right answer. We cannot, by definition, self-refer, which is NOT the case with clinicians. I’m not going to rehash that issue on this thread, but it may well be the one single reason NOT to turn over the reins of imaging to the clinicians.
Definitely a fascinating discussion, semilla! Thanks for starting the thread.