
Time to add a little color...
PACS:
1. n. (acronym) Picture Archiving and Communications System.
A device or group of devices and associated network components designed to store and retrieve medical images.
2. n. (acronym) Pain And Constant Suffering.
Sectra has been in the US for nearly ten years, and we have a superb service and support team. In addition to Philips Medical Systems, we provide Level II support for our other partners, selected dealers and comprehensive support for our direct sales.
Our PACS products for the Orthopedics and Mammography markets are extremely well received by the US market. While Philips' acquisition of Stentor will undeniably impact our revenue in the short term, we intend to aggressively bid for service on our products and continue to protect the investment of customers who have purchased Sectra PACS... whether under the Philips label or directly from us.
Sectra will continue to innovate and bring industry leading products to market in the US. If you have questions about support for your system, extensions to your Sectra PACS or have a new opportunity, we'd be happy to talk with you.
John Goble, Ph.D., President, Sectra North America, Inc. Call us at 800.307.4425.
 Today, we Star Trek fans say goodbye to James Doohan, who will be forever known as Scotty, the Chief Engineer of the Starship Enterprise. He died of complications from pneumonia and Alzheimer's disease at age 85. His ashes will be rocketed into orbit later this year. (That's not a joke, by the way; he will join Star Trek creator Gene Roddenberry, whose ashes were intered into space several years ago.) I guess we tend to forget that the characters of Star Trek are getting on up there in years. DeForest Kelly, who played Dr. McCoy, died in 1999 at age 79.
Today, we Star Trek fans say goodbye to James Doohan, who will be forever known as Scotty, the Chief Engineer of the Starship Enterprise. He died of complications from pneumonia and Alzheimer's disease at age 85. His ashes will be rocketed into orbit later this year. (That's not a joke, by the way; he will join Star Trek creator Gene Roddenberry, whose ashes were intered into space several years ago.) I guess we tend to forget that the characters of Star Trek are getting on up there in years. DeForest Kelly, who played Dr. McCoy, died in 1999 at age 79.  Even Kirk (William Shatner) and Spock (Leonard Nimoy) are in their early seventies now. I had the chance to spend 10 seconds in their presence last summer at the Star Trek convention (yes, I admit I went), while posing with my son for this photo. I call it three old Jewish guys and a kid.
Even Kirk (William Shatner) and Spock (Leonard Nimoy) are in their early seventies now. I had the chance to spend 10 seconds in their presence last summer at the Star Trek convention (yes, I admit I went), while posing with my son for this photo. I call it three old Jewish guys and a kid.
My apologies to the late Richard Harris....
I am really amazed at the traffic generated by the AuntMinnie.com article. Comments have been generally positive, usually something like, "I didn't know PACS could be funny!" I seem to have the attention of a significant number of those in the PACS community, and I would like to put that to good use while it lasts.
It seems clear that there is a disconnect between the designers and (Radiologist) users of PACS interfaces. I'm not sure why this is the case, as it seems logical to consult your end users before creating a huge software product. I don't want to indict any one particular company, but some do a better job than others of giving us the clear interface and powerful tools we need to slog through the day's work.
For the moment, lots of users, and not a few vendors are dropping by to see what foolish thing I have posted this time. Now I'm sure you all realize that is is possible for you to post comments here, and I really, really, REALLY encourage you to do so. It's simple; just click the word "COMMENTS" at the end of each posting. Perhaps this blog might be considered a "safer" place to post complaints or suggestions for the vendors, and for them to post answers. This happens on the AuntMinnie.com boards to some extent, but I think some are hesitant to post there. So, come here and let it all hang out. Don't hold back, say what you really think. I certainly haven't even begun to describe everything that would go into a perfect system, but if I can get input from as many of you as possible, maybe we can get closer to that ideal product.
Now, if you will excuse me, the boys want me to get back to the Roundtable, I mean my PACS station, and generate some revenue.
 For radiology, PACS has been nothing short of a complete and total revolution; PACS now quite literally defines how I perform my job. As a nuclear radiologist, I spend at least 85% to 90% of my day with the microphone in my left hand and the mouse in my right hand. If I'm not talking into the former whilst manipulating the latter, I'm not generating revenue for my group.
For radiology, PACS has been nothing short of a complete and total revolution; PACS now quite literally defines how I perform my job. As a nuclear radiologist, I spend at least 85% to 90% of my day with the microphone in my left hand and the mouse in my right hand. If I'm not talking into the former whilst manipulating the latter, I'm not generating revenue for my group.Since 1997, Sectra has had a global cooperation with Philips Medical Systems, which has sold Sectra's software for processing digital X-ray images worldwide.
"We have several project agreements with Philips that extend up to ten years and our cooperation will successively be terminated," relates Sectra's President and CEO Jan-Olof Brüer. "We assess that the termination will impact on our sales and earnings in the current fiscal year. At this time, however, it is difficult to provide any reliable view of the financial effects, since this depends on how much time the termination will require."
The change provides Sectra the opportunity to review its sales channels. Sectra's sales of PACS are handled on a proprietary basis in Scandinavia and other selected markets as well as through partners, of which Philips was the largest. Sectra's largest sales together with Philips have been in the US.
"Part of the sales for which Philips is currently responsible will be taken over by other partners that today are active in the same markets as Philips," says Jan-Olof Brüer. "At the same time, we gain the opportunity to advance our positions and will increase our focus on own sales in important key markets, as we do today in Scandinavia, where we have captured more than half of the total PACS market."
My answers to the above are probably predictable. First, GE and Siemens make scanners too...I don't consider the PACS product from either company, um, great at the moment. Secondly, one should never, ever make a major purchase based upon one or two perks. Would you buy a Peugot over a Mercedes because it has, say, a prettier hood-ornament? You have to take all factors into account, not the least of which is the overall usability of the entire system. Having the hots for one specific component has the potential to send you down the completely wrong path. Pull-down preliminary report generators are dandy, and I have a rudimentary version on Agfa Impax 4.5. I rarely use it, because I can type my prelim much faster without any help. As far as MPR slice thickness, I don't know anyone who finds knowing the exact numerical value of the thickness that valuable in actual use. Frankly, I suspect a lot of potential PACS purchasers, especially those who are new to the game, are so overwhelmed by whizbang gadgets, they don't stop to think about how they might actually use said toys.
My advice remains this: use the product as much as you can before making a purchase. Web-based systems lend themselves very well to trial-runs in your own office or home setting. Vendors...can you accomidate this?
Anyway. For the moment, all is well in the North Woods. That is until Sick-Call, which is right after dinner.........
Our group of 7 FTE Radiologists is in an interesting predicament. We have been using Fuji Synapse for over 3 years for in-house PACS and we are filmless for all modalities. We do a total of 140K exams a year. For the last three years our group has been pushing the hospital to provide web access to the referring docs using Synapse and they refused claiming that Synapse, outside of the intranet, is not HIPA compliant. (Synapse uses Internet explorer which can leave copies of the downloaded images on the browsing computer). So, the hospital started looking at Stentor a year and half ago. Initially we were all excited but w found out that Stentor was not able to display the Fuji CR images properly on their system. Stentor was able to fix this for new images comparisons still look pretty bad. Most radiologists also do not like the scrolling in stentor (it is too fast when you hold the mouse down or too slow to scroll one image at a time). Our referring docs are finding it a pain to navigate stentor, and clearly it is not as intuitive as Synapse. The rads want to keep Synapse and the hospital is pushing for Stentor. The rest of the hospitals in our system have gone with Stentor. (interestingly none of them have used Synapse before). Any body out there with any experience with these systems or have any general advice please post.....
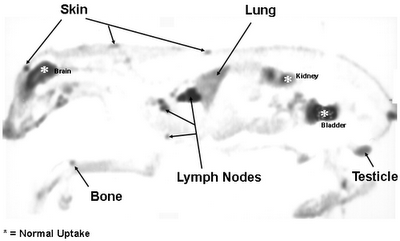 Coincidence scan of a canine, courtesy of: http://ecpi.crump.ucla.edu/vol2/issue4/matwichuk/matwichuk_case-ex.html
Coincidence scan of a canine, courtesy of: http://ecpi.crump.ucla.edu/vol2/issue4/matwichuk/matwichuk_case-ex.html
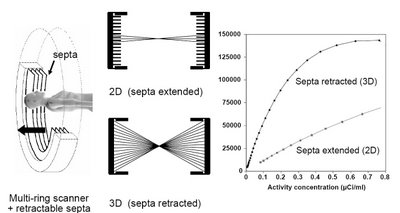
Italics are mine, as usual. Now GE cited some other articles contradicting this one. One in particular by Laritizien, et. al., states:
Comparisons of 2D and 3D performance are very sensitive to the specific conditions under which the data were acquired. Counting rate, scatter, activity outside the field of view, reconstruction algorithm, and scanner characteristics all influence relative performance. In this study 2D and 3D data were compared under clinically realistic conditions and effects that may introduce bias were minimized. The mean ratio of 3D to 2D image values was 0.94 with 95% limits of agreement of 0.63–1.41. All noise comparisons were made under conditions of matched lesion target-to-background ratio as measured in patient images. A statistically significant reduction in image noise was found with 3D acquisition compared with 2D, suggesting reductions in scan duration of 33% or more are feasible.
In this study, we performed an AFROC analysis to evaluate the impact of the acquisition mode (2D vs. fully 3D) on human observer detection performances. Three acquisition protocols were selected to provide a fair comparison between the acquisition modes. Results showed that the fully 3D acquisition mode allowed better or equivalent detection performance than the 2D mode for a same injected dose typical of the clinical practice (about 440 MBq) in a standard patient. The 2D acquisition protocol combined with higher injected doses (about 740 MBq) resulted in higher detectability than those achieved with the fully 3D acquisition mode for approximately half the injected dose. Changing the patient size or the PET scanner model will potentially change the lesion detectability results of this study.
Frost & Sullivan’s recent analysis, U.S. PET and PET-CT Markets, selected GE Healthcare as the recipient of the 2004 Market Leadership Award. This Award acknowledges the company’s exceptional marketing strategies that helped it capture the largest percentage of the U.S. positron emission tomography-computed tomography (PET-CT) market in 2003 and maintain its robust lead since the market’s inception.I have to agree 100%. GE certainly has exceptional marketing strategy. No question about that. But I don't think Frost & Sullivan is really qualified to evaluate the scanners themselves. That needs to be left to those of us who actually have to interpret the images. You might ask, "Will the Discovery fail to demonstrate something that the Biograph would show?" Now that's one question I can't honestly answer, and it's probably the most important of all. Time will tell on that one. But you can bet it will become obvious eventually.
Gee, where do I start? I hate to dignify such a posting with a response, but what the heck. I have to note at the outset that Anonymous' IP localizes him to Milwaukie, WI, the home of GE Medical systems. Coincidence? Gotta wonder... As to the rather personal comments....I would just as soon keep my name off of the blog, but my full name is revealed in the AuntMinnie article, so I am not "hiding" behind anything, thank you. If Anonymous had bothered to read some of the other entries, he would have found that I do indeed deny being in any company's pocket. Adding up all dinners and so on received from PACS vendors (which include Agfa, Amicas, Fuji, and GE) over the past five years would yield the grand total of $500. If I can be bought, it would take a lot more than that! Finally, as to my contributions to medicine, I am responsible for the introduction of PET imaging to South Carolina. Tell me, Anonymous, what have you contributed?Did you ever consider that Blogging in a medical environment would be so crude as to bash vendors. Besides, it is easy to jump on a bandwagon of the top 1, 2 or 3 with little market share and history, yet to bash others in a cowardly fashion is outright fake. What is your total combined compensation (including free meals) for promoting the top 3? Just need to know so I can budget for this when we crush them with slow steady forward progress and you turn your vote. This will remain anonymous so long as you continue to hide your identity behind an outrageous title that should belong to people to have acutally contributed something to the medical profession.
Cheers!